Make “10 in 12” a reality by monitoring the value of your physician alignment strategies

- Identifying the key elements of the physician-hospital relationship
- Defining the three essential categories of metrics necessary for valuation
- Providing examples of insights gained by combining these metrics
- Describing the human factor that is vital for success
Are you realizing the full benefit from your physician alignment strategies? Read on to find out.
Physician-hospital relationship: key elements
Since physicians are the drivers of almost all healthcare activities in both the practice and hospital setting, it’s vital to have access to the precise clinical and financial data related to such activities. Physician data is essential to coordinating and managing efforts related to providing quality patient care. Providing quality care supported by a favorable financial position requires both an in-depth understanding of care delivery and accurate cost measures of providing that care. Informing, analyzing and optimizing the efficiency of care delivery is essential to creating an enduring organization with physician and hospital alignment. Top performing health systems always include both clinicians and administrators as key stakeholders in these processes.
Physician-hospital alignment: key strategy metrics
The question is, what metrics should you use to ascertain a successful physician and hospital alignment strategy? The three main categories of metrics that define the healthcare landscape include:
1 – The Provider Network
The provider network within the U.S. is expansive with 1.2 million physicians taking part in approximately 106,000 practices. Physician work settings include about 9,000 urgent care centers, more than 4,000 short-term acute care hospitals and about 1,400 critical access hospitals. The ancillary labor force that supports these facilities is more than 5.1 million employees strong. Each provider network includes clinical and financial information. Having insights into the information that integrates physician and ancillary staff is essential for effectively managing and delivering quality healthcare.
2 – Clinical Activities
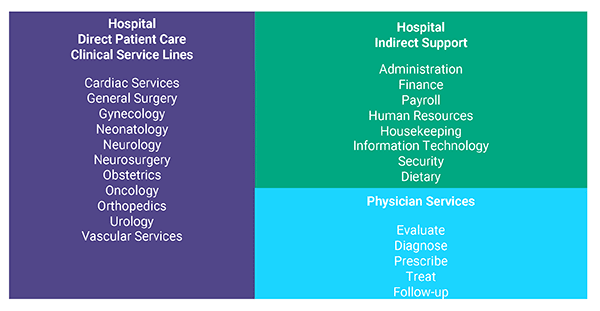
Statistical values are available from a variety of code sets that define clinical activity. They include more than 72,000 ICD10 codes, 6,900 HCPCS codes with over 300 modifiers, CPT codes and approximately 740 DRGs. To obtain a complete view of the patient encounter, it’s important to integrate detailed physician practice data with hospital service data through comprehensive service line reports. The image below highlights the direct and indirect services that encompass care delivery.
3 – Financial Data (Revenue and Expenses)
Some of the readily available metrics for financials include operating expenses, gross charges billed, payments received and insurance denial amounts. To obtain detailed metrics such as supply and labor costs or overhead expenses, you need to combine information from multiple sources and apply it to sophisticated costing models.
Gathering, defining, organizing, integrating, reporting and analyzing the data defined here is a daunting task. Having a valued strategic partner to assist with this process is an important part of accomplishing these tasks. Understanding the information that these metrics provide and their relationships is the difference between information and intelligence.
From data to insights
Having identified the key metrics of our healthcare landscape, now we need to establish a process that will move us from data to insights. We’ll use these insights to guide us in a physician-hospital alignment strategy, which includes:
- Combining disparate clinical and financial data sources
- Creating accurate, precise and detailed cost information, unique to your environment
- Delivering information from a single source with metrics to value and monitor physician alignment initiatives
The question remains: what do you do with the information and how does the result inform your decision-making process? Use the three steps below to inform and monitor your organization’s physician alignment initiatives:
- Step 1: Combine data into one place where you can apply sophisticated and flexible costing methods
- Step 2: Conduct detailed cost and profitability analysis for service lines, patient care settings and insurance plans in order to provide physicians and their groups with insights into the financial aspects of the care they provide
- Step 3: Identify outliers and define mutually agreed upon benchmarks that will support process improvement and high-quality standards
The result will be physician alignment engagements that optimize health system resources to best serve the community.
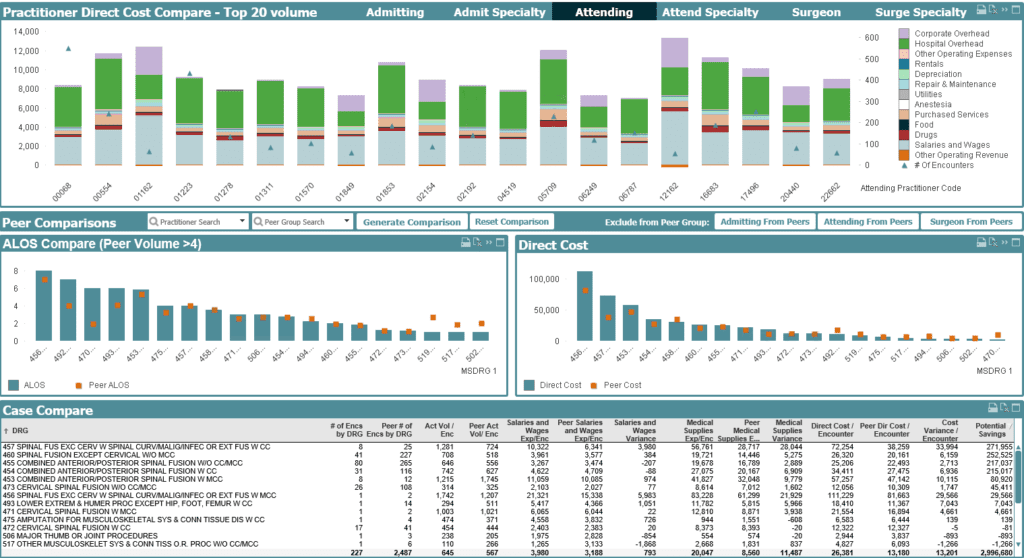
The image below shows a sample dashboard you can use to inform and monitor your physician-hospital alignment initiatives and strategy and as well as provide insights into resource utilization, process improvement and other aspects of providing quality patient care.
What can you identify by combining physician, clinical and financial data for your health system?
- Outliers related to cost of care by service line
- Cost and profitability drivers
- Practice pattern resource utilization benchmarks
- High-cost surgical implant preferences
- Direct cost of supply items that are related to quality
- Cost valuation of clinical outliers
The human factor
As a first step to meaningful conversation, hospital administrators should strive to present alignment information to physicians in an easy-to-validate format. Physicians, by relating their clinical practice knowledge to the financial information, can provide insights to the economic challenges faced by hospitals. This combination will provide everyone a clear vision to the symbiotic relationship of physicians and hospitals and its importance for a successful alignment strategy. To nurture the delicate balance of quality clinical care and to create a sustainable financial position, hospital administration should focus on resource consumption related to care delivery while respecting a physician’s autonomy to focus on providing quality patient care.
Harris Affinity’s expert healthcare consulting team has more than 35 years of experience successfully guiding healthcare organizations like yours through a complex data landscape of clinical and financial information.
Interested in learning more about physician alignment?
Join us Tuesday, June 15 for a lunch and learn where we will be digging deeper into real-world examples of physician alignment strategies and the value that our customers have experienced with us as trusted strategic partners.